What is Opioid Addiction?
You can't fight it until you understand it.
Summary:
There is an important distinction betweenaddiction
andphysical dependence
.Buprenorphine is not a treatment for physical dependence
, while it is a treatment for addiction. Understanding the difference is key to understanding and succeeding with buprenorphine.Physical Dependence
: Normal physiology expected to develop with anyone using high doses of opioids for more than a few weeks. It is resolved with a slow taper off of the opioid. People who are physically dependent on opioids will experience withdrawal symptoms if the opioid is stopped, or significantly reduced, abruptly.Addiction
: Continuous uncontrollable cravings which result in compulsive opioid use. Patients are unable to take opioids as prescribed, continue to use despite doing harm to their (or other's) quality of life. Addiction is a disorder and affects different parts of the brain than physical dependence.People who are addicted to opioids are both physically dependent and addicted
, but it is the addiction part which is the disorder. Buprenorphine treatment is for addiction not physical dependence.Understanding Opioid Addiction as a Brain Disease
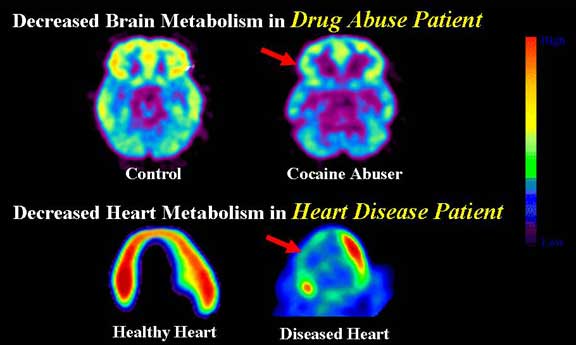
Opioid addiction is considered a chronic brain disease, because it is precipitated by fundamental, long-term, changes to the biological structures and functioning of this organ.1,2
Most brain diseases have some form of behavioral expression—Alzheimer's disease expresses itself as memory loss, schizophrenia expresses as unusual mood changes—and opioid addiction expresses itself as cravings which lead to an uncontrollable compulsion to repeat opioid use.1,3
The fact that a portion of opioid-addicted patients originally chose to misuse opioids does not make their condition any less the result of disease. Patients' choices (eg, regarding diet, exercise) contribute to the onset or severity of several chronic diseases, including hypertension, CHD, and diabetes.4
Furthermore, while the initial choice to use opioids may have been voluntary, once opioid addiction develops, use is compulsive—not voluntary.5 Although drug taking behavior can be controlled temporarily, the cravings cannot be shut off or controlled. It is the persistence of the abnormal cravings that indicates that addiction is a chronic condition.
Tolerance and Physical Dependence
The pervasive changes to brain structure and function that distinguish opioid addiction are, without exception, preceded by chronic opioid use. However, chronic opioid use is only one factor in the etiology of this disease, and, by itself, will not necessarily result in opioid addiction.3,6
Receptor molecules in the brain allow opioid molecules to attach to them which through a biological process release dopamine into the brain which is experienced as euphoria. The euphoric response may offset an existing pain condition, or if opioids are taken in the absence of pain can cause an unnaturally high euphoric response. The µ receptor has been identified as the primary opioid receptor.
Mu receptors in the brain adapt to surplus opioid-induced euphoria by becoming opioid tolerant. Tolerance is recognized as a symptom of opioid addiction, but absent of any other identifying symptoms, it is indicative only of physical dependence on opioids.3,6
As the µ receptors become tolerant to opioid drugs they also become tolerant to naturally produced opioid-like chemicals such as endorphins. The body responds by producing more of these natural opioids in an attempt to maintain a state of equilibrium.
As tolerance increases a point is reached where the body cannot produce enough natural opioids to sustain a feeling of normality and the body feels discomfort, this is withdrawal. The body becomes dependent on the external opioid supplement to feel normal. This stage of tolerance is appropriately called physical dependence and is characterized by the emergence of withdrawal symptoms upon abrupt discontinuation or substantial decrease of the opioid drug.
The desire to avoid withdrawal is not by itself an indication of addiction. Those seeking to avoid the pain of withdrawal are often mistaken for addicted drug seekers and denied necessary medication.
The neurological changes that produce opioid tolerance and physical dependence are well understood. These changes appear to correct themselves within a period of weeks following cessation of opioid use.3
Addiction is Something Different
By contrast, the cluster of symptoms recognized as opioid addiction results from neurological changes that are wider ranging and significantly more complex.3 These neurological changes do not reverse themselves shortly after opioid use has ceased, but often persist for extended lengths of time.2
The hallmark of opioid addiction—compulsive drug seeking and use—stems in large part from powerful opioid cravings brought about by these complex changes.7
Both opioid craving and opioid withdrawal frequently drive patients' drug seeking and use.3
However, only opioid cravings are tied to compulsive drug-seeking and use. Furthermore, cravings can compel compulsive opioid use independently of the presence of withdrawal symptoms or physical dependence on opioids.7
The uncontrollable drug consumption seen with opioid addiction is primarily driven by opioid cravings. This strong correlation between cravings and compulsive drug use is an inherent part of why opioid craving (but not opioid withdrawal) is considered a definitive feature of opioid addiction.7
The biological basis of drug cravings is not entirely understood much beyond the generally accepted notion that cravings are an adverse consequence of repeated activation of the brain's reward circuit initially stemming from chronic opioid use.3,7
One of the theories put forward to explain cravings posits that, over time, opioid's constant activation of the reward circuit alters neurological functioning along those pathways causing them to become "hyper-sensitized" to both the direct effects of opioids and to the environmental cues associated with their use (ie, triggers). This hyper-sensitized reward circuit causes "pathologic" cravings for opioids even in response to moderate stimulation.7
Sensitivity to opioid cravings is typically one of the most persistent symptoms of opioid addiction. This persistence is attributable to the comparatively prolonged time required for the opioid-addicted brain to restore some degree of pre-disease normalcy.2 For this reason, opioid-addicted patients may be vulnerable to drug cravings (and relapse) for months and even years after their last opioid use.7
References:
- Leshner AI, Koob GF. Drugs of abuse and the brain. Proceedings of the Association of American Physicians. 1999;111:99-108.
- Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278:45-47.
- Kosten TR, George TP. The Neurobiology of Opioid Dependence: implications for treatment. Science & Practice Perspectives. 2002;1:13-20.
- National Institute on Drug Abuse and National Institutes of Health. Lesson 5. Drug addiction is a disease—so what do we do about it? The Brain: Understanding Neurobiology Through the Study of Addiction.. Accessed April 27, 2005.
- McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment insurance, and outcomes evaluation. JAMA. 2000;284:1689-1695.
- American Pain Society. Advocacy & Policy: Definitions Related to the Use of Opioids for the Treatment of Pain. American Pain Society website. Available at: opi.areastematicas.com. Accessed September 21, 2004.
- Cam* J, Farr© M. Mechanisms of disease: drug addiction. N Engl J Med. 2003;349:975-986.